
Table of Contents

Below is an overview as to what is included on this page. This guide is here to help inform you all about eczema specifically in babies and children and to understand the different types of treatments that are available.
Topics covered:
Introduction
Eczema Pathophysiology
Types of Eczema
Eczema Treatments
Lifestyle Management
Clinical Trials and Emerging Treatments
Challenges and Future Directions
Conclusion
Introduction - What Actually is Eczema?
Eczema – also known as dermatitis – refers to a group of skin conditions that cause the skin to become itchy, red, dry, cracked and inflamed. It’s an incredibly common issue here in the UK with around 15 million of us directly impacted. For those suffering day-in, day-out with eczema flare ups and outbreaks, it can seriously affect mental health and quality of life.
The constant itching and unsightly rashes can cause stress, anxiety, trouble sleeping and low moods. It’s no wonder a recent survey by the National Eczema Association found that over 30% of respondents felt like eczema controlled their lives.
Eczema can start early, often affecting infants before their first birthday. These poor little ones end up puffy-faced and blotchy, incessantly scratching which can then lead to painful open wounds and infections. As a parent, it can be very upsetting to see a child in constant discomfort and distress.
You may also be all to familiar with the exhaustion that comes from night after night of broken sleep trying to stop babies scratching themselves raw. So why, if it causes such suffering, is eczema so prevalent? Well that’s the billion pound question. Fact is, there are still gaps in the research when it comes to the precise causes.
What experts do know is that eczema tends to run in families and is linked to overactive immune systems and inflammation. There are various types too, depending on symptoms and suspected triggers.
Atopic eczema – the most common form – often develops alongside other allergy-related conditions like asthma and hay fever. This suggests it originates from within and may have genetic factors.
Contact eczema – occurs as a reaction when skin touches certain substances. Common culprits include detergents, cosmetics, metals like nickel, and other irritants like wool fabrics. Even stress levels – as well emotional states – are thought affect some suffers.
Clearly it’s complicated, which is precisely why managing the condition can be so frustrating. When a flare strikes it seems to have a domino effect, setting off the dreadful itch-scratch cycle. As hands furiously graze the inflamed patches, the skin ruptures leaving it vulnerable to nasty bacteria. Yet resisting the urge to claw and rub the burning areas proves virtually impossible. For kids it’s especially tough as they lack restraint and can end up damaging their often fragile skin. Which parent hasn’t helplessly watched their child transform into a wild, unstoppable scratching machine? It’s awful knowing this will only amplify the situation but not knowing how to make it stop.
The options to ease things seem endless yet also inadequate or short-lived. There are now over a dozen various ointments, eczema creams and prescribed potions such as steroids for reducing inflammation and combatting infection. Bleach baths – as horrid as they sound – may temporarily relieve areas after deep scratching. Wet wrap bandaging can enable topicals to better penetrate. Then there are systematic treatments like immunosuppressants and newly developed biologic injections to dampen down haywire immune responses. Not to mention elimination diets in case allergies play a role, antihistamines, special silk clothing to avoid irritants… the list goes on.
But still, eczema continues to plague families at staggering rates so whether any of this is truly helping long term is debatable. The fact most medical guidance focuses on reacting after the damage is done highlights how little is still understood. What’s evidently needed is more investment in research around preventative approaches. Perhaps if causation – rather than just symptom reduction – becomes the target, this distressing condition can eventually be contained. In the meantime, the millions stuck relentlessly riding the eczema rollercoaster will surely agree – serious progress can’t come soon enough!
Eczema Flare Ups
Whilst experiencing a flare up can be traumatic, even patient support systems seem inadequate. Social media groups provide some sense of community for sufferers who often feel isolated and embarrassed about appearances. But these quickly become flooded with (usually well-meaning) amateurs dishing out reams of unqualified advice. Recommendations range from simply drinking more water to scissors for desperate parents forced into altering distraught children’s fingernails. Some even suggest sufferers haven’t explored healing crystals or probiotics enough! And photos of weeping skin and bloodied bedsheets trigger widespread horror and panic amongst members. So whilst bringing eczema out of the shadows is positive, the reality of living with it day-to-day remains trivialised.
Evidently so much more empathy, understanding and proper help is needed. Starting perhaps with wider public health messaging about the severity of the condition. Society tends to still perceive it as a bit of benign dry skin. Annoying yes, but not generally debilitating like other chronic issues. Phrases like ‘oh just put some cream on it’ or ‘have you tried moisturising’ continue making the rounds. If 15 million UK citizens were instead losing sleep, battling anxiety and living in physical anguish because of persistent joint pain or migraines, more would surely be done. So a wider appreciation of the true impacts eczema has on people’s wellbeing and what that means is key. Only then can those trapped scratching through night after night finally stop feeling so dreadfully alone. And with some luck, future generations may be spared from this agonising and misunderstood condition altogether.

Eczema Pathophysiology
Deciphering precisely what triggers the onset of eczema has perplexed dermatologists and allergy specialists worldwide for decades. Unlike many common skin conditions, eczema cannot be traced back to one single origin or cause. In fact, ‘the eczemas’ would be a far more fitting label for this group of frustratingly enigmatic inflammatory skin disorders.
The Immune System and Eczema
What experts do know is that in patients with eczema, something has gone awry to disrupt the immune system’s usual balance. Rather than performing controlled reactions to perceived threats, it starts to overreact and sets off unnecessary inflammatory cascades. These then manifest as irritable, angry rashes on whatever skin areas are targeted.
Genetic factors clearly enable this immune dysfunction. Twin studies demonstrate that if one identical twin has atopic dermatitis (the most common eczema subtype) the other twin has a 75% likelihood of developing it too. Compare this inheritance pattern to non-identical twins, and that likelihood plummets to 15-20%. This strongly implicates variations called polymorphisms amongst human leukocyte antigen genes are partly accountable. These genes are integral for regulating immune responses but slight mutations mean responses spiral out of control.
Whilst inheritance confers susceptibility however, genetics cannot be solely to blame. Otherwise 100% of identical twins would be afflicted. Here is where environmental elements gain relevance. Exposure to different allergens, bacteria or even emotional situations seem to essentially ‘trip the switch’. They activate dysfunctional immune cells to suddenly flood into tissues and spawn inflammation.
Scientists now recognise this two-hit concept of genetic disposition being met with environmental catalyst helps account for eczema’s origins. It also explains the perplexing variability patients endure. Long periods of seemingly healthy unblemished skin become interrupted by abrupt flares of raw, blistered skin. Then these outbreaks mysteriously vanish again, often without any change in external factors.
Delving deeper into the immune pathways eczema exploits further elucidates its development. Skin mast cells for instance usually remain inert until roused into action defending against injury or pathogens. But in eczema patients they malfunction, perceiving benign targets like dust mites or pollens as dangerous intruders. Incited by immunoglobulin E, they violently trigger the release of histamine and other inflammatory messengers.
Nearby tiny muscles lining microscopic pores then contract in response, obstructing vital secretions meant to hydrate the skin surface. Sweat and sebum become trapped beneath forming the perfect breeding ground for troublesome microbes like Staph bacteria to spawn infection. Immune cells once again flood the area but struggle containing these opportunistic bacteria. The ensuing debris and pus physically tears the skin barrier allowing allergens deeper access to spark further reactions.
Thus the notorious ‘itch-scratch’ cycle relentlessly propagates. Nerve fibres detecting the continuous immune signalling grow hypersensitive. They start firing excessively to adjacent nerves making previously innocuous touches or clothing brushes feel unbearably itchy. Unable to tolerate the sensations, patients instinctively scratch and open blisters which further intensifies chemical and microbial exposure. Their now utterly overwhelmed immune systems perpetuate massive waves of inflammation as this self-perpetuating loop continues.
Clearly multiple interconnected networks spanning genetics, immunology, neurobiology and environmental science all participate to propagate eczema. Like an elaborate domino rally, as one component topples it collides with the next ultimately ending in the catastrophic widespread tissue destruction eczema represents. Whilst no universal cure exists yet, recognising these intricate chains of events is galvanising more strategic treatments.
Monoclonal antibody injections for example directly intervene by binding up excess immunoglobulin E antibodies before they interact with mast cells. Stem cell educator therapy first extracts and ‘reeducates’ defective immune cells then returns them to circulation to behave properly. Such targeted treatments appreciating the precise pathophysiological pathways offer new promise. They demonstrate that slowly but surely, the elaborate inner workings underpinning the eczemas are starting to be revealed.
Yet despite these encouraging steps, huge unanswered questions persist around what initially corrupts immune functioning in the first place. If doctors could pinpoint precise genetic discrepancies or environmental elements that critically switch eczema on, targeted prevention may finally be possible. For now though, patients have little choice but to reactively manage whatever symptoms may come their way.
This essentially leaves them playing a perpetual game of roulette, anxiously hoping their number won’t come up at the next spin. When rashes do flare, desperately trying to calm the tide of inflammation again feels fruitless. Still the itching and oozing continues regardless, with sleepless nights and stained sheets that come with it. Exhausted parents watch infants morph into unsettled bundles of weeping skin night after night. Teenagers avoid social activities from embarrassment over visible rashes. Adults juggle never-ending medical appointments and trials of various ointments all amidst fatigue and despair. This is the grim reality for so many families weathering this devastating condition.
Clearly aside from physical agonies, the psychological impacts cannot be overstated either. Research increasingly shows higher incidences of depression, anxiety and poor self-esteem in eczema patients. Body image issues frequently develop in adolescents whilst younger children often struggle academically and behaviourally. Strained parental relationships plus financial losses from work absences or medical bills all add further dimensions too.
Yet doctor sympathy remains mixed according to patient reports. Some feel dismissed as overly anxious hypochondriacs. Others sense frustration from physicians out of solutions and forced to merely offer more ‘band aid’ solutions without ever addressing root causes. What patients unanimously do value however is empathy around the true burdens eczema creates. They need clinicians willing to hear their fears, validate their spiralling loss of hope and partner with them. Only through openness, compassion and continued scientific revelation can headway finally be made against this devastating scourge.
Types of Eczema
When it comes to eczema, it’s not a case of simply having ‘the condition’ or not. In fact this is an umbrella term encompassing numerous different skin afflictions all classed as eczema but with their own unique set of features. Understanding these distinctions is crucial as treatment plans vastly differ based on whichever version patients find themselves saddled with. Let’s delve into the most prevalent subcategories of eczema recognised today and what sets them apart from one another.
Atopic Dermatitis (AD)
The poster child for eczema, atopic dermatitis is by far the most widespread type making up over two thirds of cases. Usually starting in childhood, dry irritated patches crop up that are intensely itchy and inflamed. Common zones include elbow creases, wrists, knees, ankles and the neck area. Many kids eventually do ‘grow out’ of AD yet for others (this author included!) it persists lifelong with intermittent flares. AD also tends to run alongside related atopic conditions like asthma and hayfever.
Contact Dermatitis
This eczema variant occurs directly following skin contact with specific substances. Like atopic dermatitis it creates angry red, weeping rashes but localised to affected areas. Common triggers are chemicals like bleach, metals like nickel in jewellery, fragrances, plants like poison ivy or everyday products like detergents. Avoiding culprits is key yet identifying them amidst our chemical-laden world can be tricky. Patch testing helps confirm diagnoses. Management centres around barrier protection creams alongside vigilance around personal products and environments.
Dyshidrotic Dermatitis
Targeting hands and feet, stubborn blisters define dyshidrotic dermatitis often followed by peeling, cracks and cuts. Outbreaks tend to cycle through periods of dormancy and recurrence rather mysteriously. Potential triggers include seasonal allergies, emotional stressors, metals and chemicals. Potent steroid creams may relieve bouts along with infection prevention. Yet the elusive nature of dyshidrotic flare ups remains poorly understood making them hugely frustrating.
Seborrheic Dermatitis
Contrary to its name, this eczema variant has no links to oil secretion disorders like acne. Instead inflammation affects oil-rich zones like the scalp, face, upper back and groin. Skin gets greasy and scaly with stubborn dandruff often accompanying scalp flares. It shares similarities with psoriasis and fungal infections, hence topical antifungal medication is often the first port of call alongside gentle skincare regimes. Managing flare factors like stress is recommended yet predictably outbreaks equally strike spontaneously.
Nummular Dermatitis
Here distinct coin-shaped lesions develop, most frequently on lower legs. These itchy plaques often emerge following an injury which later become eczematous. Dryness and a perpetual cycle of scratching and infection propagates the patches. Potent anti-inflammatory creams help calm flare ups whilst exclusion of irritants allows recovery. Lesions however often persist and reopen at the slightest friction making nummular dermatitis particularly stubborn.
Clearly recognising which type of eczema patients have is pivotal for appropriate care. Referrals to allergy specialists or dermatologists allow formal diagnoses based on presentation, medical history and investigative patch tests. Patients can then trial specific treatment pathways suitable for their form alongside identifying individual flare triggers.
For example, if contact allergies or irritants frequently spark outbreaks then obviously minimising exposures is wise. Those vulnerable to emotional stressors equally must implement self-care strategies to endure stressful periods. Other cases may warrant systemic immunosuppressants or biologic agents to rein in haywire immune responses. Climate factors like extreme cold for some individuals makes winter sun escapes advisable too!
Equally understanding eczema tends to morph over time prevents false assumptions around causes and treatments. What begins as suspected atopic dermatitis might evolve into nummular patches later or alternate between types randomly. Patients may require flexible regimens to accommodate changing features.
Clearly no singular approach fits all and any universal ‘cure’ remains wishful thinking. Yet through patients and doctors closely collaborating to decipher specific drivers behind each eczema variation, management can be better tailored. This offers the greatest chances of containing the condition as best possible – even if some guesswork around the unpredictable beast eczema represents will always be required!
Beyond these commonly discussed subtypes, various other rare eczema variants exist too. Discoid eczema features round lesions much like nummular dermatitis but occurs predominately on the trunk, arms and legs of adults. Photo-exposed eczema flares up only where sunlight contacts the skin as with other light-sensitive dermatoses. And asteatotic eczema arises on areas lacking sebaceous glands like shins when moisture is depleted. Diagnosis difficulties mean exact prevalence is unknown however.
Pediatricians meanwhile recognise additional eczema phenotypes more unique to infants. Neonatal and infantile eczema for example often spontaneously develops within days or weeks of birth before sometimes resolving. Distinctive features like nipple eczema in breastfeeding babies helps discrimination from conditions like scabies or psoriasis also common in early life. Tailoring skincare routines to delicately balance cleansing whilst preventing dryness is key. Topical steroids still remain controversial in tiny babies so milks and emollients are emphasised first.
Then there’s the complex topic of skin colour impacts on eczema diagnosis and care. Those with darker tones often report greater disease severity yet experience delays receiving therapy. Underlying health biases around black and brown skin seemingly still pervade dermatology too. Consequently community-led initiatives are fighting for better eczema understanding and funding for ethnically diverse groups.
So clearly amidst the many subtypes and nuances separating eczema classifications, one fact remains consistent. Raising awareness for this highly complex, changeable and often debilitating condition must persist across all sectors of medicine. Only through continued public discourse can the extra patient supports and research breakthroughs so desperately needed finally gain more well-deserved traction.
Eczema Treatments
When facing the misery of an eczema flare-up, most patients try everything and anything for even a hint of relief. Yet amidst the staggering array now available, deciding what solutions may lessen symptoms (and what will make them worse!) proves overwhelming. Add to that many therapies lacking robust clinical data, and no wonder sufferers feel utterly confused in a crowded marketplace.
In this guide we’ll simplify the key evidenced options starting with standard first-lines then overview some common ‘alternatives’. The golden rule however is maintaining realistic hopes – this notoriously unpredictable condition rarely follows textbook pathways. But through methodical trials plus good doctor-patient communication, quality of life with eczema can undoubtedly still improve.
Topical Treatments
Managing eczema fundamentally relies on restoring and protecting the skin barrier using emollients and medicated creams. These provide simple, safe and effective at-home care across mild to moderate cases. Proper usage holds the greatest impact so education around when and how to liberally apply is pivotal.
Emollients
Whether gels, ointments or lighter lotions these all serve to hydrate, moisturise and trap existing skin moisture. Forming a protective barrier also limits future water loss whilst allowing other medicated options to better penetrate when layered underneath. Opt for fragrance/perfume free formulas and use frequently even after skin seems healed to maintain flexible, healthy tissue.
Steroid Creams
These tackle inflammation which triggers eczema’s vicious itch-scratch cycle. Judicious short-term use controls flare-ups effectively yet fears over skin thinning means guidelines suggest intermittent rather than continuous usage. Mild hydrocortisone (1%) sold widely treats limited patches but stronger clobetasone or betamethasone formulas obtained on prescription better target widespread severe cases.
Calcineurin Inhibitors
Similar anti-inflammatory effects as steroids but without skin thinning side effects makes these a possible maintenance therapy. Tacrolimus and pimecrolimus cream both reduce immune reactions and inflammation although burning or stinging can occur initially. Their exact long-term safety remains under investigation however hence reservation around use in young children.
Antibiotic Creams/Ointments
When weeping skin becomes cinnamon coloured and crusty, bacterial superinfection has likely occurred. Over-the-counter antibacterial creams containing chlorhexidine provide local action against colonising staphylococci and streptococci species. Anti-itch creams with menthol, calamine or crotamiton also sometimes offer short-term relief.
Systemic Treatments
If topical measures and avoidance of individual triggers fails to control eczema or coverage is too extensive, systemic therapies target the immune dysfunction. These treatments however carry higher risks thus require specialist dermatology oversight around use.
Oral Steroids
Powerful pills like prednisolone rapidly reduce inflammation and symptoms when eczema suddenly flares out of control. Strict short-term limits of around 7-10days exist however due to immunosuppression risks allowing infections alongside other harmful metabolic effects long-term. Pulse therapy with intermittent higher dosing may treat acute episodes without the same cumulative side effects of daily regimens.
Oral Immunosuppressants
Medications like ciclosporin, methotrexate, mycophenolate and azathioprine dial down faulty immune reactions through differing mechanisms. This prevents flare factors like allergens triggering cascades of inflammation underlying eczema flares. Lengthy blood monitoring accompanies these meds evaluating liver health and cell counts. Plus the aimed ‘controlled state of immunosuppression’ increases risks of low immunity hence vigilance for infections is vital.
Biologic Injections
The newest systemic class specifically targets runaway immune messengers shown to drive allergic diseases. Dupilumab for example binds up free interleukin 4 and interleukin 13 cytokines whilst other emerging biologics have additional mechanisms. Administered via regular subcutaneous injections, these show remarkable efficacy in eczema without suppressing wider immunity. Some patients report almost complete disease remission! Cost and questions around long-term use however currently limits their availability.
Phototherapy
Controlled repeated exposure to certain wavelengths of ultraviolet light has anti-inflammatory and immune-dampening effects in the skin. Both narrow band UVB lamps or UVA plus psoralen tablets followed by UVA exposure helps around 70% of patients not responding to usual treatments. 2-3 sessions a week for 6-12 weeks are typical during flares alongside ongoing maintenance exposures. Yet published studies are fairly outdated and access inequitable across NHS clinics. Moreover longer term melanoma risks from repeated UV likely exists.
Complementary Therapies
Growing frustrations around eczema’s unpredictability explains why more holistic avenues constantly beckon patients. Acupuncture, homeopathy, herbalism, oils and supplements all claim success yet quality evidence is scarce. In fact some natural concoctions actively worsen skin irritation. However as safe adjuncts to enhance quality life complementary therapies have merit. Just ensure consulting registered practitioners rather than well-meaning but ill-informed amateurs!
Dietary Approaches
Many naturally attempt eliminating various foods in case allergies or intolerances trigger eczema flares. Common culprits are dairy, eggs, wheat or high histamine produce. Stricter gut healing protocols like GAPS or paleo diets also help some patients. Blood testing checks for actual allergies whilst food diaries identify suspect items. Supervision by nutritionists however ensures dietary needs stay met if excluding entire food groups long-term.
Probiotics/Prebiotics
Links between gut and skin means nourishing healthy gut flora shows promise managing skin inflammation. Probiotic strains like lactobacillus rhamnosus GG are especially well studied. They reduce histamine production and dampen immune reactivity amongst other protective mechanisms in eczema patients. Prebiotic plant fibres that act as fertilizers for our microbiome community likewise show benefits.
Essential Fatty Acids
Clinical trials using evening primrose, borage, blackcurrant seed or fish oils show some reduction in inflammation and dryness associated with eczema. Anti-inflammatory omega-3 fatty acids help repair skin cell structure and lock in moisture when consumed regularly. Opting for cold-pressed oils may retain greater potency yet standardisation between products warrants better regulation.
Herbal Remedies
Traditional plant preparations utilising naturally occurring phytochemicals and compounds target various eczema drivers. For example Mahonia ointments containing berberine reduce bacteria and inflammation. Chamomile, liquorice and calendula creams protect against irritants and allergens by strengthening skin barrier proteins. Herbs however have known drug interactions making transparency around their use essential.
The Mind-Skin Connection
Given stress notoriously aggravates eczema, addressing psychological facets offers huge quality of life improvements. Meditation, self-hypnosis, yoga, nature-based or art therapy all help redirect nervous system responses away from pro-inflammatory pathways. Counselling sessions additionally teach cognitive skills preventing anxiety and depression worsening flares. Multipronged holistic care should target the whole patient not just bothersome skin!
Clearly no panacea yet exists amidst eczema’s complex web of subtypes, triggers and symptoms. But through open-minded, responsive, patient-centred care the illness burden can assuredly be lessened. Clinicians that appreciate using evidence-based integrative tools alongside alternative avenues provide that additive support. They understand treatment means more than just never-ending unsuccessful prescriptions. It requires building trust, validating struggles and improving wellbeing beyond the constraints of broken skin…
Clothing / Fabrics
When choosing fabrics, opt for soft, breathable materials like cotton and silk whenever possible. They tend to be less irritating than rougher options such as wool. Consider clothes made of lightweight linens or smooth cotton blends if you need warmth but find wool itchy.
It’s also helpful to wash new garments before wearing them. Sometimes manufacturing processes leave behind chemical residues or stiffening agents that haven’t been fully rinsed out. Give your clothes a gentle wash to remove any irritants and ensure comfort.
And don’t forget the little details that could cause discomfort! Snip off tags, especially any near your neck or inner wrists where they might scrape sensitive skin. Seek out seamless constructions if seams tend to bother you. The smooth finish helps prevent red marks and chafing.
Following these tips will help you build a wardrobe gentle on sensitive skin. Focus on soft, breathable, pre-washed essentials whenever you can. With some care in selecting and preparing items, you can stay cozy and comfortable no matter the weather or activity.

Designed to bring them comfort
For maximum comfort, the garments include off-set, flat seams to ensure minimal irritation.

Healthy skin is HappySkin®
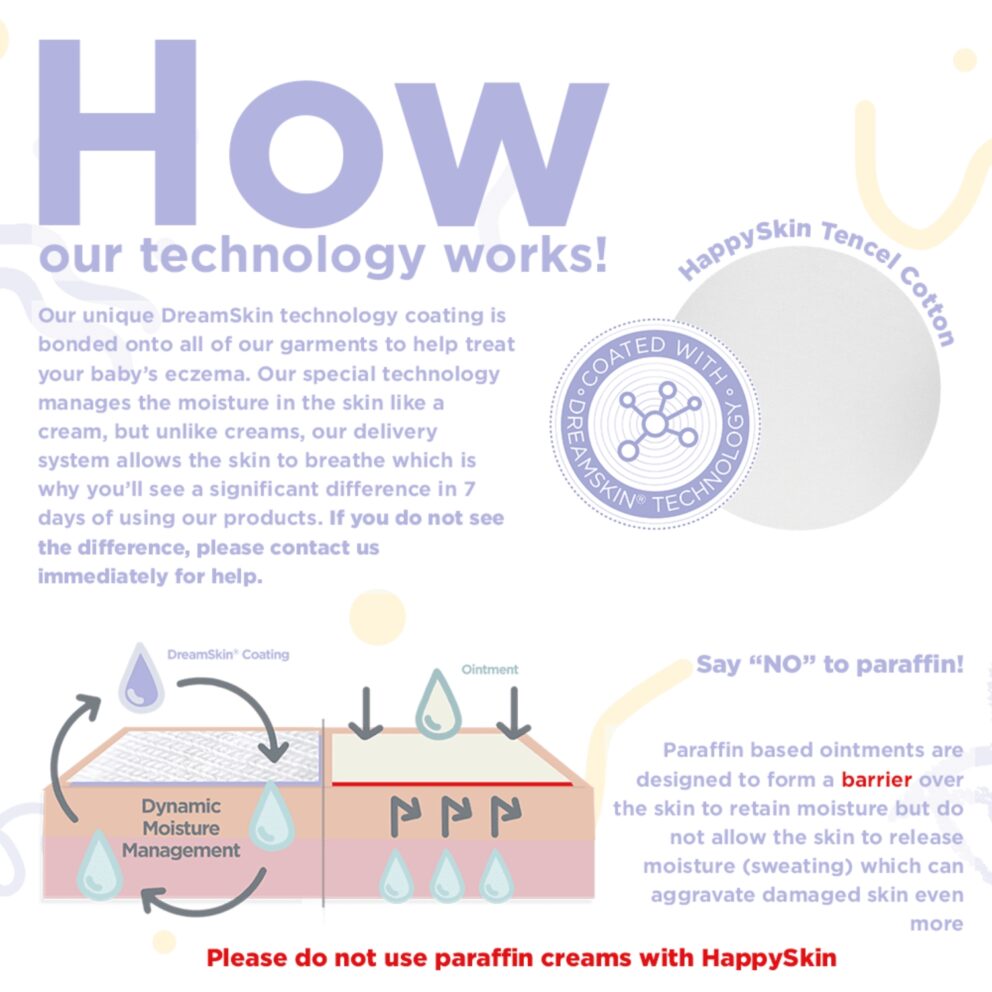
HappySkin is a range of base layer clothing, which are designed to be worn next to the skin.

Protection for your little ones
HappySkin forms a next-to-skin barrier to provide protection against skin irritants often found in washing detergents, which can lead to further irritation.
Our products
As any eczema veteran knows, caring for this fickle condition extends way beyond pots of cream and medication regimens. Like playing a perpetual game of niggling roulette, what aggravates skin today brings no flare tomorrow and vice versa ad infinitum. Hence patients – and parents of little sufferers – must become vigilant detectives constantly evaluating potential triggers. Because whilst no definitive eczema cure exists yet, minimising lifestyle factors provoking symptoms can make life far more bearable.
Establishing solid skincare foundations, identifying and avoiding personal flare triggers then reducing stress form the essential trifecta for successful self-management day-to-day. Add on a healthy diet, activity levels and skin-friendly wardrobe choices too for that extra advantage. So let’s explore these key areas in greater depth and how families can implement positive changes without it totally overtaking life!
Skincare Routines
Once diagnosed, request referral to skin therapy specialists that educate patients about suitable cleansing, moisturising and medication regimens. Showering or bathing techniques preventing moisture depletion is pivotal – short lukewarm showers with mild cleansers like aqueous cream best. Pat drying then immediately applying liberal emollients and/or prescribed topicals further bolsters the damaged moisture barrier. Ointments containing petroleum provide occlusion overnight whilst lighter creams suit daytime. Reapplying these after wet work or hand washing also maintains skin integrity.
Customising routines for different body parts proves important too. For example, eyelid eczema warrants delicately formulated gels to avoid eyes whilst nappy regions need zinc oxide barrier protection from urine and faecal enzymes. Scalp flare ups conversely may benefit from medicated shampoos containing coal tar, salicylic acid or antifungal ketoconazole. Such tailored modifications reduce irritation, infection risks and better control troublesome areas.
Schools and childcare centres should be informed about suitable cleansers andcustomised soap free wash routines too. This prevents well-meaning staff inadvertently aggravating skin through improper exposures to irritants. Clear written instructions outlining specific emollients, timings and procedures helps minimise issues.
Trigger Identification
Meticulously tracking potential environmental or internal contributors triggering outbreaks provides immense insight informing management. Numerous options for recording daily activities, exposures plus diet alongside symptom changes now exist. Simple paper diaries noting flare patterns help identify potential weekly, monthly or seasonal influencers. Meanwhile smartphone apps allow easy photo documentation and reminders evaluating suspected source elimination.
Common sparks include new products, pets, pollen or infections. House dust mites, moulds and staphylococci bacteria rank as perennial villains too. Then there’s the fun realm of seemingly random stress-induced flares that cruelly erupt pre-big meetings, weddings or holidays! Comparing readings illustrating weather conditions like low humidity and skin changes also highlights ‘at risk’ scenarios. So don’t ignore the detective work – it reaps informative dividends!
Healthy Lifestyle Basics
Ensuring adequate sleep, balanced nutrition and exercise might sound mundane but all bolster immunity resilience. Lowered defences from run-down bodies exacerbate inflammation so don’t underestimate their value. Additionally build in ample downtime for enjoyable activities that de-stress. Reading, crafts, gentle walks outdoors (with sun protection!) all enhance wellbeing. Basically nurturing overall health equates to nurturing skin health with eczema!
Dietary Considerations
Elimination diet trials temporarily excluding suspect foods offers useful diagnostic confirmation around triggers. Dairy, eggs, nuts, soy, seafood, gluten and high histamine produce like berries, tomatoes or avocados all commonly aggravate. Yet long-term restrictions require planning to prevent nutritional shortfalls or eating disorders in kids. Registered nutritionists and allergy testing help guide reintroduction phases determining tolerance thresholds. Once known, adjusting eating patterns accordingly may lessen intermittent flares without restrictive diets.
Additionally ensure adequate intake of foods containing antioxidants, essential fatty acids and phytonutrients. These compounds help control inflammation levels plus build healthy cell membranes. So filling shopping trolleys with colourful veggies, oily fish, nuts and seeds makes perfect dietary sense with eczema!
Family Help & Emotional Support
Enlisting household help around trigger modification advice proves invaluable for families. Demonstrating suitable laundry techniques, identifying irritant cleaning products or perfecting moisturising routines means the whole team works together mitigating exposure. Outlining specific chores broader friends and family can assist with like meal trains further alleviates pressures too.
Most importantly however, kids and parents alike require ample emotional validation around this stressful lifelong condition. Connecting with in-person or online support groups to share frustrations often comforts like no textbook advice from physicians can! It powerfully reassures families they are neither alone nor hysterical as they courageously navigate eczema’s relentless rollercoaster… And that shared empathy ultimately makes each difficult day facing unpredictable flares that little bit easier.
The take home for families? Firstly approach eczema as a team effort – it greatly bolsters resilience. There’ll be bumps (and flares!) along the way but through collaboration, education and self-advocacy victories emerge. Expecting instant fixes masks the chronic reality of eczema. But focussing efforts around protective lifestyle factors, trigger avoidance and emotional health undoubtedly proves most rewarding long-term. Essentially when eczema cannot be controlled, lifestyles can transform to accommodate it better instead!
Wider Societal Shifts Needed
Whilst equipping patients and families with bespoke management advice offers progress, change equally needs to occur across broader sectors too. For example, schools simplifying uniform codes encouraging comfortable cottons over scratchy woollens makes perfect sense for student inclusion. Meanwhile teachers should receive basic eczema first aid like avoiding shaming kids with visible rashes given psychological harms. Edutaining classmates about triggers and the functional impacts through puppet shows or relatable stories fosters empathetic peer relationships too.
Stronger regulation around cosmetic and skincare marketing warrants attention as well. The rise of ‘clean beauty’ brands arrogantly shames tried and tested mainstay products like parabens as ‘toxic’. Yet no sound evidence corroborates claims preservatives trigger allergies or eczema flares in humans at tiny usage levels. On the contrary for sensitive groups, heavily stunted preservative-free products pose far higher infection risks! Ceasing scare-story influencer promotions surrounding everyday essentials could protect vulnerable populations.
Construction industry reforms additionally require prioritising health in housing standards. Factors like humidity, ventilation, mould and pollutants inside buildings hugely influence respiratory conditions alongside eczema. Tighter legislation enforcing minimum energy-efficient insulation requirements plus stricter damp and toxin testing during rentals or renovations therefore proves vital.
Finally from a medical perspective, improved eczema awareness in primary practices is pivotal. Too often patients report frustration around delayed referrals, misdiagnoses or dismissive attitudes over symptoms. Lessons outlining characteristic rashes, common trigger questions plus basic first line instructions around emollients allows swifter, appropriate care. Meanwhile bulk prescription rights in community pharmacies prevents constant battles obtaining adequate topicals.
So whilst day-to-day self management rests with patients, collective responsibilities for enabling healthier environments exist. Through coordinated public health efforts right across interlinking industries, the extreme eczema burden across hundreds of thousands of Britons need not remain quite so heavy indefinitely. But it requires society recognising the true extensive impacts eczema poses within families and communities before transformative action gains traction.
Challenges & Future Directions
Frustrated faces fill dermatology waiting rooms nationwide as eczema continues inflicting miseries upon millions despite the 21st century’s medical prowess. Devastatingly for patients, impactful solutions easing the incessant itch and subsequent mental anguish remain tauntingly out of reach. So where exactly do obstacles rest impeding meaningful progress against this painful, pervasive skin scourge? How might we overcome them to restore normalcy for affected individuals and families suffering unrelentingly year upon year?
Insurmountable Treatment Hurdles
Interestingly, treatments with proven efficacy do exist for controlling eczema reasonably well in many scenarios. But several common barriers conspire preventing patients benefitting optimally from their transformative effects. Issues around therapy access, adherence, convenience and affordability mean too few endure the intended game-changing gains documented in research findings.
Access Difficulties Abound
Consider phototherapy for example – a well validated UV light regimen easing symptoms in around 70% of patients resistant to standard treatments. Yet clinics providing this specialised facility remain scant across regions despite demand, with byzantine referral procedures limiting access further. Consequently applicants face extensive waiting lists eventually having to commute significant distances repeatedly… an impossible ask already struggling work-wise and financially from eczema’s functional impacts.
Similar access problems initially plagued emerging injectable biologics as well. Phenomenal trial outcomes revolutionising prognoses saw dupilumab fast-tracked for approval in serious cases. But gaining NHS prescriptions proved near impossible at first with doctors denying referrals altogether having never heard of these novel agents! Gradually expanding uptake together with patient advocacy group pressures now improves the situation but barriers undoubtedly persist for innovative therapies.
Treatment Hassles Deter Engagement
Assuming therapies reach patients appropriately, challenges around exhausting regimens frequently undermine engagement too. As an example take topical steroids – first line defence against flares yet notoriously troublesome to use effectively. Their specified ‘consistent application thinly only to affected areas’ proves almost farcically impossible when entire bodies erupt angrily. Sleep-deprived parents frantically slathering writhing infants or independent adults contorting to plaster backs know well the messy realities!
Eventually treatment exhaustion sets in amidst the ongoing slog of messy procedures and mountains of soaks, creams and bandages. So unsurprisingly, 50% of parents report difficulties persuading children to comply with skin directed therapy. But even motivated older patients confess forsaking intricate routines occasionally to preserve some illusion of normalcy and autonomy. Such intentional non-adherence seems entirely reasonable considering treatment itself starts disrupting living detrimentally. Yet skipping obviously risks aggravating issues further – an unfair choice no one should face.
Prohibitive Personal Costs
Assuming therapies miraculously become easily accessible and simple to follow, for too many households their annual expense still positions them out of reach. After all, standard moisturisers and medications plentiful enough to use liberally cost several hundred pounds annually even before any supplementary items! Out of pocket costs therefore run thousands yearly once additional therapies come into play, representing major proportions of overall incomes for lower-earning families.
Eventually difficult choices around food, heating and rent arise when budgets remain overwhelmed by relentless eczema costs. Some parents even report needing to select which one out of multiple affected children receives treatment in any given month – an appalling tragedy no first world country should ever inflict upon desperate families! Clearly pricing structures around managing chronic illnesses desperately requires better arrangements enabling equitable financial access.
Future Progress Possibilities
So multiple complex interlinking factors limit treatment effectiveness daily despite best medical intentions. But possibilities certainly exist for overcoming such hindrances impeding eczema care through coordinated efforts between healthcare services, political powers and patient needs. Technology and innovation themselves continue favourably disrupting therapeutic spaces as well.
Streamlined Care Pathways
Centralising specialised multi-disciplinary care units catering holistically to eczema could better support patients regionally. These hubs incorporating medical dermatology alongside psychology, nutrition, social assistance and pharmacy guidance under one roof means personalised needs get addressed efficiently. Currently families frustratingly duplicate their story across fragmented services that insufficiently communicate about cases. By contrast, integrated centres encourage consistent practitioner relationships for overall wellbeing beyond just skin. Digital health records enhance this through data sharing securely across linked services as well.
Political Momentum
Raising eczema higher on political agendas remains imperative progressing policies aiding families and empowering workforces too. Campaignspublicising true symptom burdens help build urgency around the condition whilst updated teaching syllabuses guarantee new graduates enter practice equipped managing cases. Advocating inclusion of emerging therapies on NHS formularies also prevents outdated practices lagging behind the latest medical capabilities. With coordinated pressure from doctors, patients and scientists collectively lobbying governments, legislative transformations supporting eczema can assuredly gain traction.
Innovative Solutions
Apps allowing customisable reminders for recommended regimens could make adhering with treatment simpler in everyday contexts. Smart moisturiser dispensers and electronic wands tracking usage meanwhile give clarity around whether sufficient amounts get applied for best results. We see technology revolutionising so many spaces so why not clever innovations supporting self management as well? Teledermatology with remote consultations via video messaging further eases burdens reaching specialist care.
Exciting Progress in Drug Developments Too!
Novel delivery mechanisms now enable topical medications reaching deeper skin layers for enhanced absorption whilst minimising application volumes needed. Small proof of concept trials using nanocarriers, liposomes and crystal mesh sheets containing active drugs showcase early promise delivering drugs through the intact barrier. Patients could soon feasibly target source inflammation precisely rather than relying solely on superficial anti-symptom effect creams.
Systems furthermore automatically adjusting therapy strengths responsive to disease activity markers represent another avenue nearing reality. Periodic biomarker testing assessing patient immune response profiles determines customised tweaks of drug doses, combinations or timing that could revolutionize precision. Gene expression patterns indicating exactly which immune pathways drive someone’s eczema form the basics enabling this approach.
The Bottom Line?
Collaborative efforts between health sectors, politics, patients and disruptive technologies can absolutely overcome frustrating therapeutic limitations haunting today’s eczema patient. Through creative solutions improving convenience, access, costs and overall education around the illness itself, life-changing treatments need no longer exist exclusively in theory. The potential now clearly rests in innovative hands to transform that theory into daily tangible reality – where potent eczema treatments finally reach their destiny benefitting ordinary people needing them most.
Future Treatments
For eczema patients fruitlessly trialing every moisturiser and ointment imaginable, breakthroughs in clinical research finally offer new hope. Novel therapies that target the intricate immune malfunctions underlying eczema rather than just temporarily easing symptoms are progressing rapidly. These range from new formulations of existing medications right through to bespoke treatments leveraging individual patient genetics. So let’s review some positive steps forward that could revolutionise outlooks for this burdensome condition.
Novel Topical Options
Improving potency, safety and application methods of common topical treatments remains an active focus in pipelines. New steroids with alternative mechanisms aim to maintain efficacy whilst minimising skin barrier damage associated with traditional formulas for example. These additionally explore combining anti-inflammatory action alongside antimicrobial, antifungal and antipruritic (anti-itch) activity within singular creams or gels.
More attention concentrates on calcineurin inhibitor immunosuppressants like pimecrolimus too. Trying longer-term use to prevent recurrent flares rather than short bursts during outbreaks has returned promising results so far. Paediatric populations struggling with frequent symptoms especially benefit as normally reservations around rare skin cancer risks restrict prescription in the young. Novel vehicles like foams, impregnated wipes or micro-emulsion sprays better suit delicate facial areas as well compared to thick ointments prone to itchy eyes.
Additionally ‘soft’ over-the-counter options based on nanotechnology, lipids and peptides aim to rebuild the skin barrier safely during remissions. These cutting edge options may help maintain periods of disease control according to emerging trial data.
Oral and Injectable Options
Despite initial fanfare, disappointing sustained responses to initial oral immunosuppressive medications like methotrexate or azathioprine plague the field. Biologic agents however represent an exciting new class with dupilumab leading the way. This injectable monoclonal antibody binds inflammatory messenger proteins interleukin-4 and interleukin-13 shown to drive multiple allergic responses including eczema. Patients receiving regular doses report rapid improvements in symptoms, quality of life, plus reduced flare frequencies over time.
Several other monoclonal antibodies now entering large scale testing take precision targeting to the next level. They home in on specific cell surface or signalling proteins responsible for immune cell activation and migration towards the skin specifically. Early efficacy signals look very positive with improved adverse effect profiles compared to immune-suppressing alternatives.
Phototherapy Developments
Ultraviolet light therapy traditionally requires inconvenient repeat visits to specialist clinics with concerning cumulative skin cancer risks. Now newer targeted phototherapy attempts localising treatment just around active eczema lesions using fibre-optic cables. These deliver patterns of UV light tailored to individual flare areas identified via thermal imaging cameras. Home-based devices give patients autonomy managing outbreaks day-to-day as well. Though mostly still experimental, accessibility advances like these positively expand options beyond medications alone.
Future Personalised Directions
Eczema’s varying severities between patients with similar characteristics underlines its complex heterogeneous nature. Excitingly, decoding genomic signatures and gene expression patterns from tissue or blood samples now explains differing responses at the individual level. These molecular insights pinpoint exact immune pathway dysfunctions genetically predisposing people to eczema subtypes alongside predicted triggers and medication compatibilities too.
Soon such sequencing could determine personalised treatment selections and optimal timing of therapies that specifically correct the aberrant biological processes identified. This approach termed ‘precision medicine’ thus ensures the right interventions get delivered to the right patients. It certainly beats fruitless symptom-chasing trial and error tactics that dominate currently!
Whilst eczema afflicts millions unrelentingly today, never before has research momentum achieved such monumental strides. Harnessing futuristic patient-specific genetic data alongside advanced targeted treatments at last make prevention, proper control or even total cure potentially imaginable. What hopes these latest developments offer restoring normal functioning skin and quality of life for the numerous individuals and families tired of bandaging up the daily devastation eczema delivers!

Conclusion
After extensively reviewing myriad facets around living with and treating eczema, several takeaway messages come to light that deserve underscoring. First and foremost, the necessity for greater empathy, understanding and urgency around eczema cannot remain understated from a societal stance. This truly devastating condition still receives too little medical priority or community awareness despite imposing colossal suffering upon millions nationwide.
As our explorations uncovered, quality existence becomes painfully compromised when skin – our major protective organ against the world – fails so catastrophically. Victims young and old endure far more than merely superficial symptoms from eczema’s wrath. The ripple effects through destroyed sleep, daily activities, relationships, mental health and finances for families proves incredibly far-reaching. Yet dismissal or misconceptions around the depth of these functional impacts persists across all sectors.
From sidelined research funding and disjointed healthcare pathways to inadequate clinical teaching and support resources – tragic shortfalls fail patients at multiple inflection points. Stark health inequalities still disproportionately disadvantage minorities battling eczema too. Plus divisive beauty norms heaping shame around visible skin conditions fuels the crisis. Essentially the unnecessary loneliness and distress persisting amidst eczema stems as much from cultural dismissiveness surrounding the illness as it does the torturous flares themselves.
Progress positively shines too though – we cannot ignore the incredible leaps in scientific revelations around this previously mystifying condition. Right from decoding the intricate immune and genetics underpinnings perpetuating symptoms through to trailblasing biologics tackling specific culprit pathways, momentum builds gaining momentum. Translating these vital laboratory breakthroughs into clinical implementations that actually benefit patients does demands dedicated coordination between stakeholders however.
Fortunately precedents across other therapy spaces highlight that dismantling access barriers around emerging treatments proves possible over time through tenacity and collaboration. We see initially prohibitively expensive drugs for rare diseases become funded through health policies that eventually recognise their efficacy. Patient lobby groups similarly hold sway progressively driving political parties prioritising previously ignored conditions too. So whilst monumental challenges exist, history shows that with coordinated pressure, the eczema field can assuredly transform as well.
Building urgency firstly requires collective acknowledgement of how profoundly the eczema problem currently controls and destroys the lives of far too many within our local communities. Only once treated as an urgent crisis warranting crisis-level responses can services, policies and societal norms shift gear away from the wholly inadequate status quo patients presently endure.
Through our extensive discussion unpacking eczema’s numerous facets, hopefully now sufficient context illuminates just why ‘simply using another cream’ fails spectacularly addressing this issue for most. We realise how multifaceted drivers from environment through genetics, psychology and skin biochemistry steamroll into the disastrous symptom rollercoaster patients ride relentlessly. Appreciating this complexity subsequently highlights why singular solutions typically flop and frustration understandably brews.
Yet despite eczema’s multiple intersecting cogs proving impossible to control outright, our journey uncovered how carefully navigating management can still transform outlooks. Defining patterns around individual disease behaviour does empower patients reclaiming aspects of life eczema continually snatches away. Cautious avoidance around understood triggers, structured skincare foundations and building bodily resilience shields against some fluctuation at least. Such self-care flair and fortitude undoubtedly forges greater certainty amidst eczema’s notorious uncertainty.
But admitting the exhaustive reality existing with eczema even during periods of ‘control’ remains crucial as well. Often the invisible battles patients fight nonstop to simply keep heads above the tide go unseen, whilst the dramatic flares attract disproportionate attention. In truth however, the relentlessness pressing on with skin regimes, lifestyle measures and medical appointments impedes normalcy just as much in the calm. Facing this frustrating monotony saps motivation yet receives so little empathy from clinicians or community accordingly.
Eczema’s unpredictable chaotic nature explains why scientifically decoding its precise biological basis so critical as well – only then can management evolve from crude reactive crisis control into targeted prevention strategies. Breakthrough laboratory findings highlighting recently defective skin barrier proteins, immune messengers and gene expression gone array finally provides those answers! The eczema field now hasidentified culprits perpetuating inflammation rather than just attempting temporary symptomatic relief futilely.
Building on such monumental genetic revelations, the era of precision medicine promises customised approaches specific to aberrations identified in individuals too. Rather than fruitless trial and error around dozens of creams or supplements hoping one miraculously sticks, objective testing determines tailored recommendations. These aim correcting the core dysfunction promoting eczema in patients rather than chasing inflammation surface levels alone. Whilst still partly conceptual, pilots demonstrate eczema therapy informed by gene data cuts six-fold more symptom days than standard guidelines.
Maturing innovations in specialised phototherapy, nanotechnology drug delivery and microfluidic testing kits further widen the possibilities improving care. Technology holds incredible capacity circumventing conventional frustrations patients face as well. Creative adhere once devices monitoring usage, telehealth access portals and 3D printable brace solutions all feature on the horizon!
So in summary, monumental leaps behind the scenes position the eczema world at a pivotal junction. Science now provides foundations enabling radically strategic interventions whilst public momentum urges prioritising support and resources accessibly. Of course barriers stand strong and stakeholders must unite dismantling them if patients today still subsisting needlessly are to ever feel change. But armed with greater awareness of eczema’s true devastating impacts together with emerging tools revolutionising outlooks, perhaps the tide could turn for coming generations instead. This future promises integrated services, multimodal therapies tailored to individuals and societies accommodating rather than alienating visible skin disease.
For today’s unrelenting sufferers, such visions may seem optimistic pipedreams amidst their daily turmoil and isolation. Yet their involvement vocalising struggles to powers spearheading alterations can help precipitate that shift. We owe building this realm of understanding, compassion and innovation to the broken individuals and families robbed of life and liberty by eczema thus far – they above all deserve restored hope. What seemed for decades just a bothersome itch now has opportunity through awareness and answers to no longer remain the destructive, misunderstood scourge stealing life quality for millions…..
For further reading on newborn eczema treatments – click here








